6 Sepsis Nursing Care Plans. Updated on October 13, 2023. By Paul Martin, BSN, R.N. Make use of this in-depth nursing care plan and management guide to aid in the care of patients with sepsis. Expand your knowledge base of nursing assessments, interventions, goal setting, and nursing diagnoses, to meet the distinct needs of patients with sepsis. Sepsis is a systemic infection and requires close monitoring of vital signs with prompt intervention. Nurses must recognize patients at risk for developing sepsis and prevent a worsening of their condition. Nursing Diagnosis: Risk for Infection. Related to: Immunosuppression ; Multiple chronic comorbidities ; Compromised skin or tissue integrity

Our popular sepsis infographic has been updated to reflect the hour1
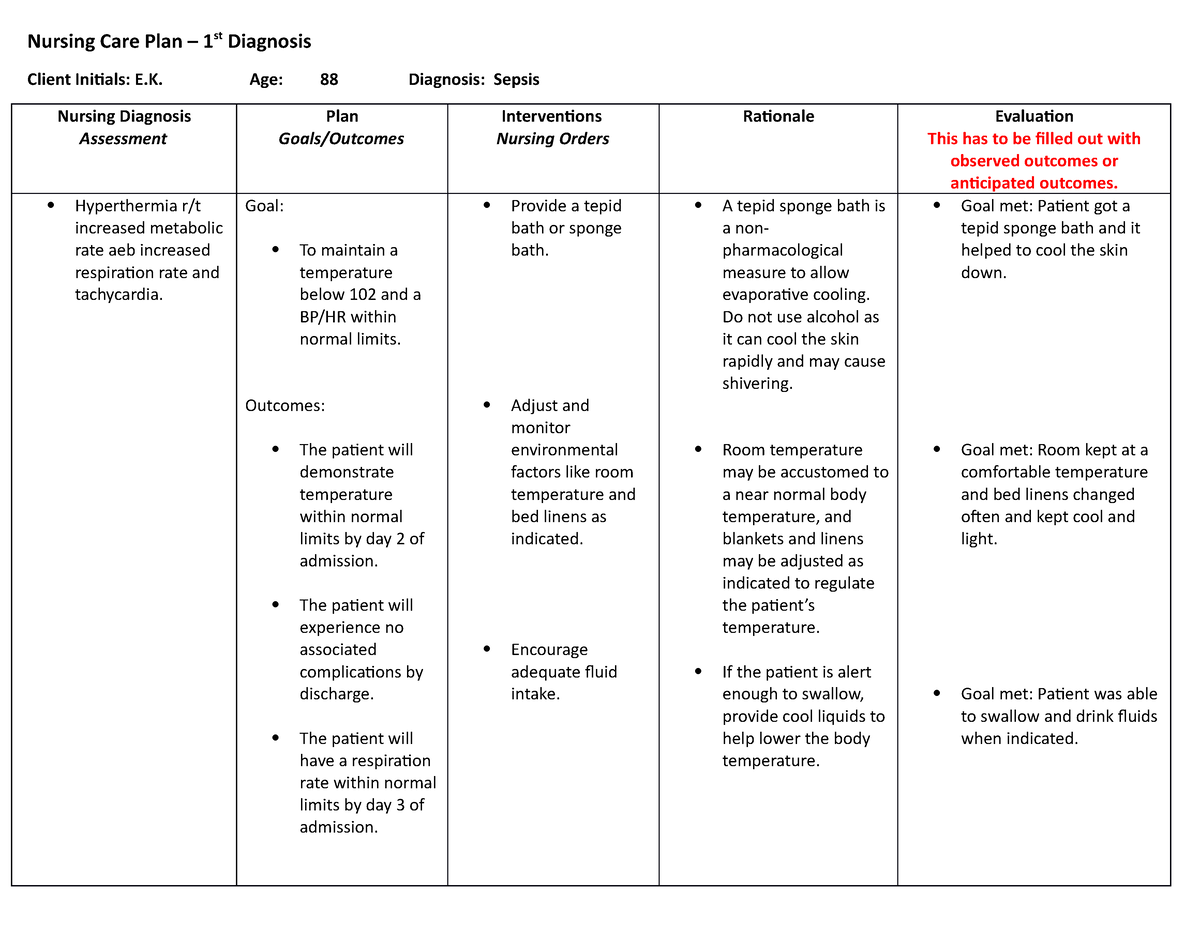
Nursing Diagnosis for Sepsis Nursing Care Plan for Sepsis 1. Nursing Diagnosis: Hyperthermia related to sepsis secondary to severe pneumonia as evidenced by temperature of 38.5 degrees Celsius, rapid and shallow breathing, flushed skin, profuse sweating, and weak pulse. This article aims to highlight the critical importance of nursing in battling sepsis and septic shock, shedding light on the pathophysiology, risk factors, clinical presentations, and evidence-based interventions.. Diagnosis. Sepsis can affect a lot of body systems and even cause their failure, so diagnosis is an important part of the. Sepsis is a substantial global health burden and is the leading cause of death among adults in intensive care units (ICUs). 1 It affects more than 900,000 people annually in the United States. Nursing Diagnosis for Sepsis. When diagnosing a client with (possible) sepsis, look for signs of infection (e.g., fever, chills) AND either evidence of systemic inflammation or hypoperfusion.. Nursing Actions & Care Note for Sepsis. Nurses are the first point of contact for clients with sepsis, and their actions can greatly impact a client.
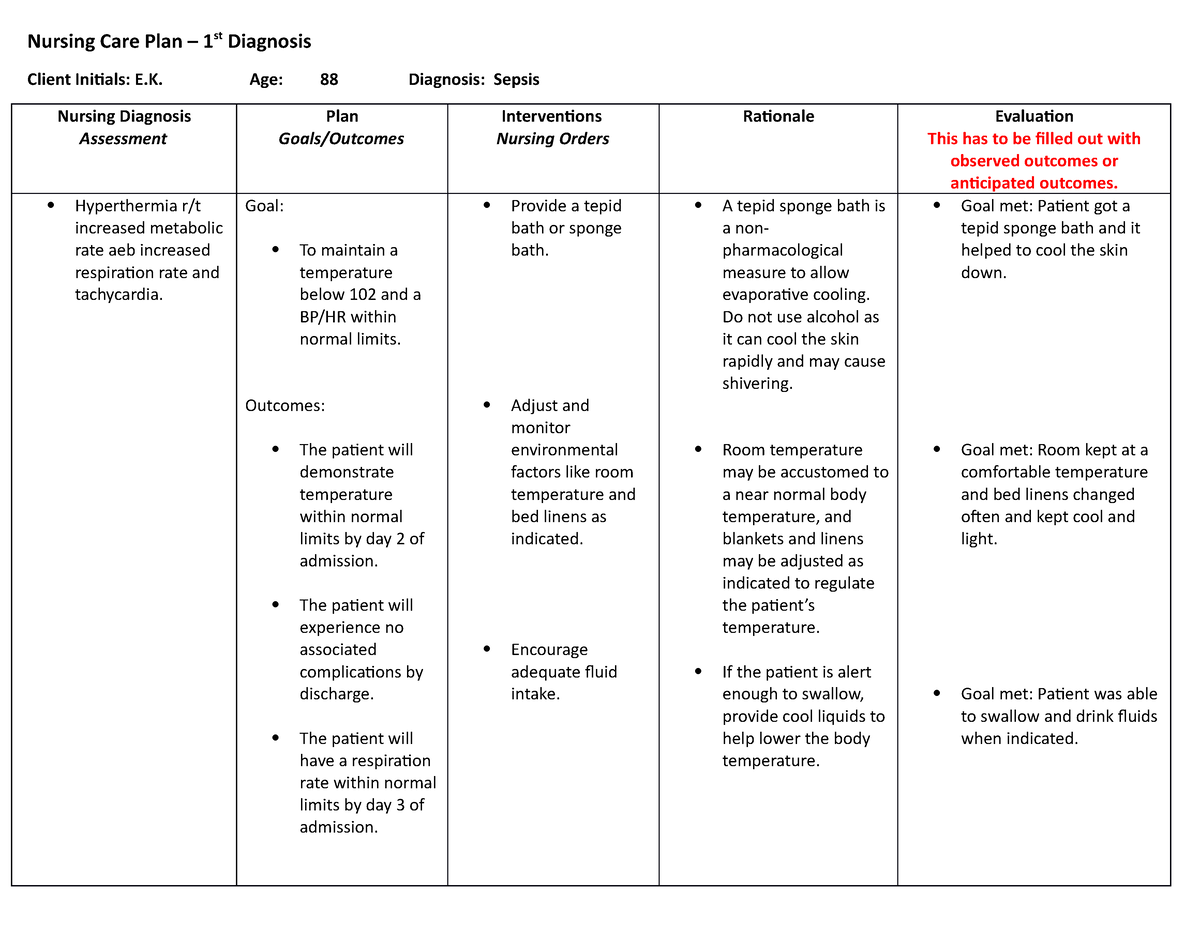
Sepsis Nursing CARE PLAN Nursing Care Plan 1st Diagnosis Client
INTRODUCTION — Sepsis is a clinical syndrome characterized by systemic inflammation due to infection. There is a continuum of severity ranging from sepsis to septic shock. Although wide-ranging and dependent upon the population studied, mortality has been estimated to be ≥10 percent and ≥40 percent when shock is present [].In this topic review, the management of sepsis and septic shock. Nurses on the Front Line of Sepsis. Sepsis is the #1 cause of death in the U.S. and accounts for about 6% of acute care admissions each year. It is also the #1 cause of readmission to acute care facilities, with a 90-day readmission rate of nearly 40%. On average, approximately 35% of patients diagnosed with septic shock do not survive. Nursing Assessment for Sepsis. Regularly monitor vital signs, including temperature, heart rate, respiratory rate, and blood pressure, to identify signs of systemic inflammatory response and monitor response to interventions. Assess for clinical signs of infection, such as localized redness, swelling, warmth, and pain. Process: 1. Al residents/patients with a confirmed or suspected infection wil be screened for sepsis using SIRS criteria. 2. If a resident/patient with a confirmed or suspected infection meets two or more SIRS criteria, the Sepsis Nursing Protocol wil be implemented by the registered nurse (RN). Protocol: 1.
Sepsis Nursing Care Plan Tutorial YouTube
Nursing Diagnoses for Sepsis (NANDA International, Inc., 2018; Doenges, et al., 2014) The chance of survival from sepsis depends on the early detection of problems and accurate diagnosis to formulate an efficient timely nursing care plan and implement immediate life-saving interventions. Nurses play a fundamental role in detecting changes in physiological observations that could indicate the onset of sepsis. Additionally, an awareness of the pathophysiology of sepsis allows the nurse to better understand how rapid intervention prevents the onset of septic shock. Furthermore, knowledge and use of clinical guidelines and sepsis.
Sepsis syndromes span a clinical continuum with variable prognoses. Septic shock, the most severe complication of sepsis, carries a high mortality. In response to an inciting agent, pro-inflammatory and anti-inflammatory arms of the immune system are activated in concert with the activation of monocytes, macrophages, and neutrophils that interact with the endothelium through pathogen. The Sequential Organ Failure Assessment (SOFA) score is a tool used as an objective measure of organ dysfunction in critical illness, including sepsis. 4 A SOFA score of 2 or more points from the patient's baseline is abnormal and indicates an increased mortality risk. 2,4 The CDC has published an electronic SOFA tool (eSOFA) that can be used.

Updated definitions of and clinical criteria for diagnosing sepsis and
Bacterial sepsis is a life-threatening condition that arises when the body's response to an infection injures its tissues and organs. Sepsis has recently been re-defined as life-threatening organ dysfunction caused by a dysregulated host response to infection.[1] Sepsis, as a medical condition, was first introduced by Hippocrates (460 through 470 BC) and is derived from the Greek word sipsi. Nursing Care Plan for Sepsis. June 5, 2023. 91590. Sepsis ( 1) is scary. It can start off showing signs and symptoms of pneumonia, urinary tract infection or the flu. Before you know it, it has already developed into a widespread inflammation and infection, causing organ failure and even death. As a nurse, it's your responsibility to ensure.