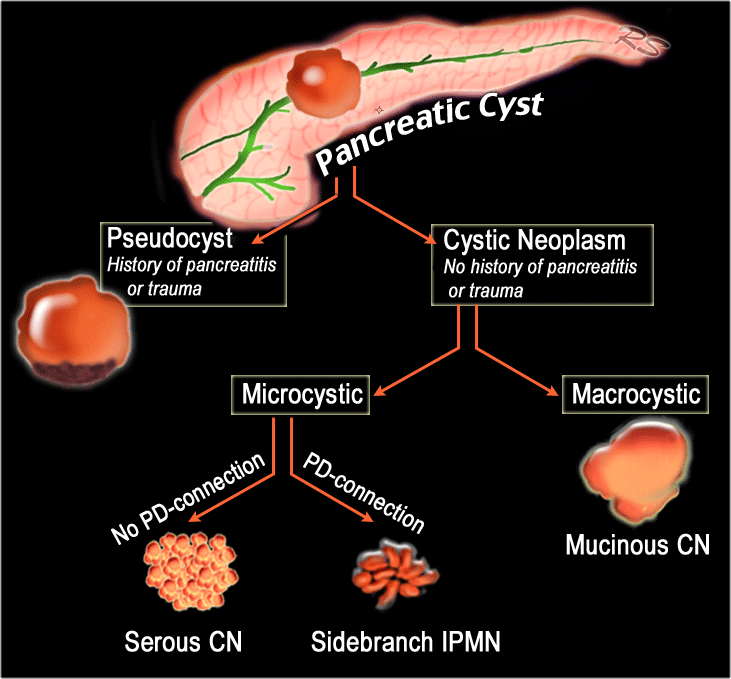
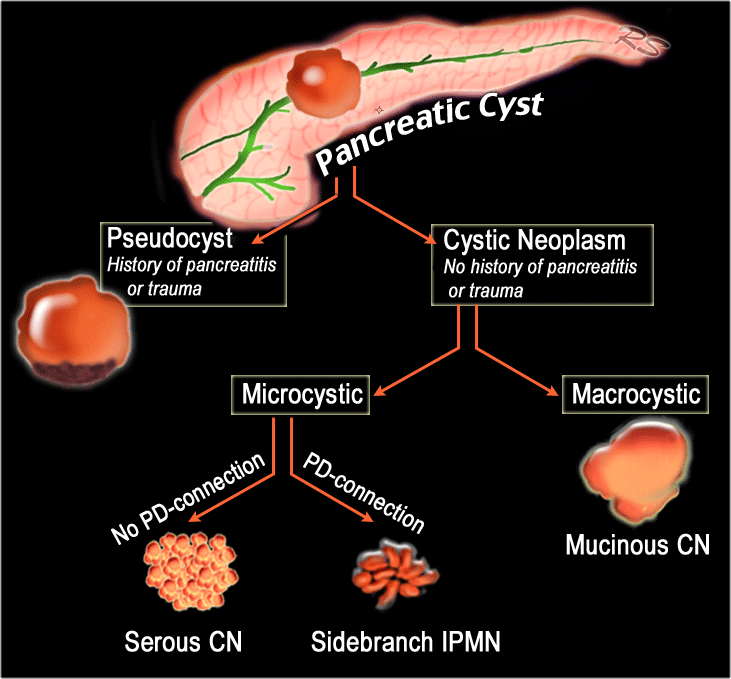
Introduction Classification Pancreatic cysts can be categorized into the following groups: Pseudocysts Common cystic neoplasms: IPMN - intraductal papillary mucinous neoplasm SCN - Serous cystic neoplasm MCN - Mucinous cystic neoplasm Uncommon cystic neoplasms: SPEN (solid pseudopapillary epithelial neoplasm) Tumors with cystic degeneration: The core objectives of the Incidental Findings Project are to (1) develop consensus on patient characteristics and imaging features that are required to characterize an incidental finding; (2) provide guidance to manage such findings in ways that balance the risks and bene fits to patients; (3) recommend reporting terms that re flect the level o.
The Radiology Assistant Pancreas Cystic Lesions
Pancreatic cystic Lesions. Radiology department of the Academical Medical Centre, Amsterdam and the Alrijne hospital in Leiderdorp, the Netherlands. Cystic pancreatic lesions are increasingly identified due to the widespread use of CT and MRI. Certain pancreatic cysts represent premalignant lesions and may transform into mucin-producing. Publicationdate 2021-08-01. This is the second version of the role of CT in staging pancreatic cancer. Pancreatic cancer is the fourth largest cause of cancer death in the United States and Europe with over 100,000 deaths per year in Europe alone. The overall 5-year survival ranges from 2-7 % and has hardly improved over the last two decades. glucagonoma cystic teratoma metastases to pancreas Retroperitoneal lesions (extrinsic to the pancreas) can mimic pancreatic cystic lesions, when close to the gland. Examples include: cystic lymphadenopathy (e.g. necrotic) duodenal diverticulum CME Tools Share Abstract The widespread use of high-spatial-resolution cross-sectional imaging has led to an increase in detection of incidental pancreatic cystic lesions. These lesions are a diverse group, ranging from indolent and premalignant lesions to invasive cancers.

The Radiology Assistant Pancreas Cystic Lesions
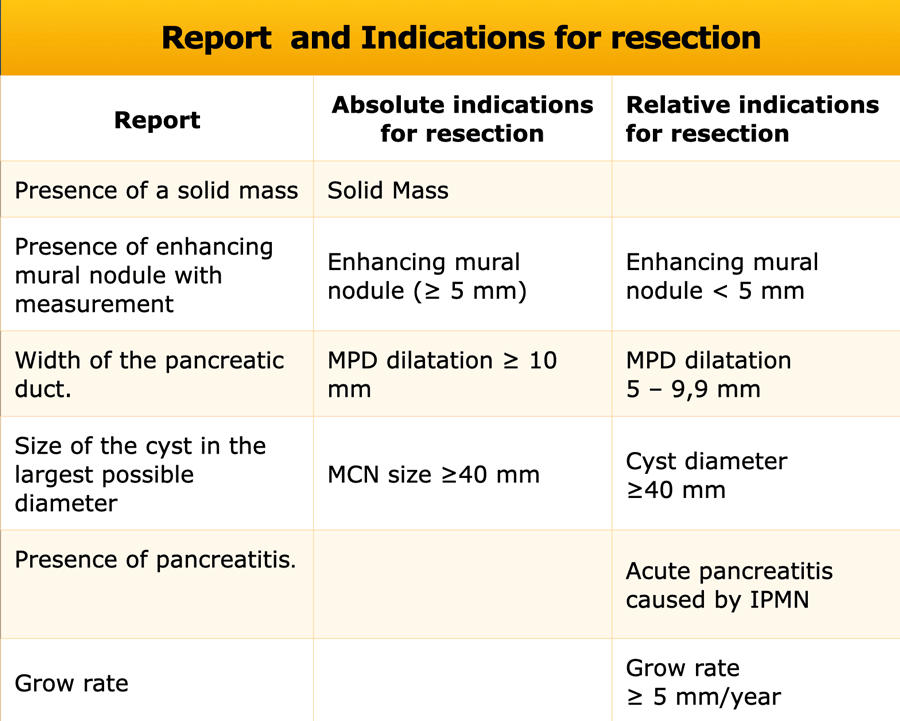
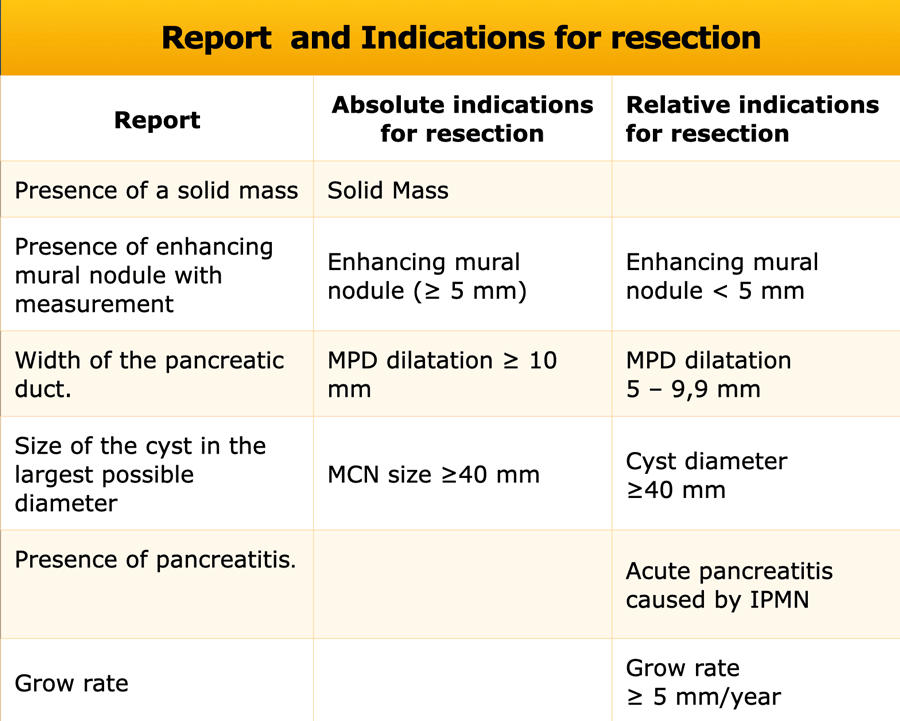
The purpose of this review is to outline the management guidelines for the care of patients with cystic pancreatic lesions. CONCLUSION. The guidelines are as follows: Annual imaging surveillance is generally sufficient for benign serous cystadenomas smaller than 4 cm and for asymptomatic lesions. Computed tomography and magnetic resonance imaging are excellent modalities for both initial detection and characterization of cystic pancreatic lesions. An imaging classification system for these lesions has been proposed that is based on the morphologic features of the lesion. Introduction. Cystic pancreatic lesions (CPLs) are quite common: Their frequency of detection ranges from 2.4 to 19.6%, and their prevalence as well as size and number increases with age (from 7.9 below 70 years to 40.2 over 70 years) [1-5].A precise characterization is fundamental for the correct management of these lesions, as they have heterogeneous biological behavior and different. Cystic pancreatic lesions (CPLs) are frequently casual findings in radiological examinations performed for other reasons in patients with unrelated symptoms. As they require different management according to their histological nature, differential diagnosis is essential. Radiologist plays a key role in the diagnosis and management of these lesions as imaging is able to correctly characterize.

The Radiology Assistant Pancreatic cystic Lesions
The most common cystic lesions of the pancreas seen on imaging are pseudocysts, serous cystadenoma, mucin-containing lesions (IPMN, mucinous cystadenoma, or cystadenocarci-noma), and solid papillary epithelial neoplasm. Other rare pancreatic cystic lesions include true epithelial cysts, cystic islet cell tumors, and adenocarcinoma with cystic. OBJECTIVE. The purpose of this review is to outline the management guidelines for the care of patients with cystic pancreatic lesions. CONCLUSION. The guidelines are as follows: Annual imaging surveillance is gener-ally sufficient for benign serous cystadenomas smaller than 4 cm and for asymptomatic le-sions.
microcystic serous cystadenoma: usually head; 30% have a central scar cystic with a solid component macrocystic tumors can have a solid component as well pancreatic adenocarcinoma may undergo cystic degeneration (8%) 6 generally solid Introduction Temporally, two phases of acute pancreatitis are identified in the Revised Atlanta Classification: Early - first week Only clinical parameters are important for treatment planning and are determined by the systemic inflammatory response syndrome - SIRS, which can lead to organ failure. Late - after the first week
The Radiology Assistant Pancreatic cystic Lesions
Abstract. Although the probability of pancreatic cystic neoplasms (PCNs) being detected is raising year by year, their differential diagnosis and individualized treatment are still a challenge in clinical work. PCNs are tumors containing cystic components with different biological behaviors, and their clinical manifestations, epidemiology. Pancreatic cystic lesions are relatively common imaging findings and may be secondary to both benign and malignant disease processes. Accurate characterization of the internal features of a cyst—including fluid, hemorrhage, septa, and enhancing soft-tissue components—is important to guide the differential diagnosis, and cross-sectional magnetic resonance (MR) imaging is the optimal.