Close Health Treatments, Tests and Therapies Hospital Discharge What is hospital discharge? When you leave a hospital after treatment, you go through a process called hospital discharge. A hospital will discharge you when you no longer need to receive inpatient care and can go home. In most cases, a hospital discharge form is the only document that accompanies a patient to the next stage of medical care. Well-written discharge summaries are typically considered important when promoting safety when a patient transitions between care settings, especially during the initial post-hospital period.
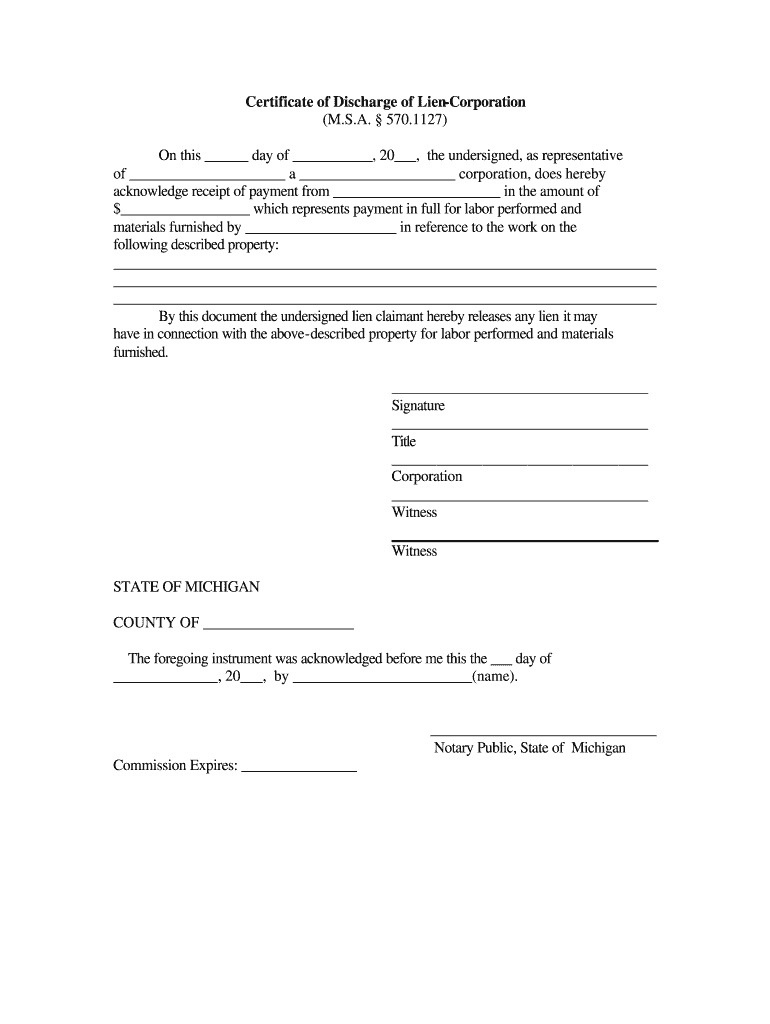
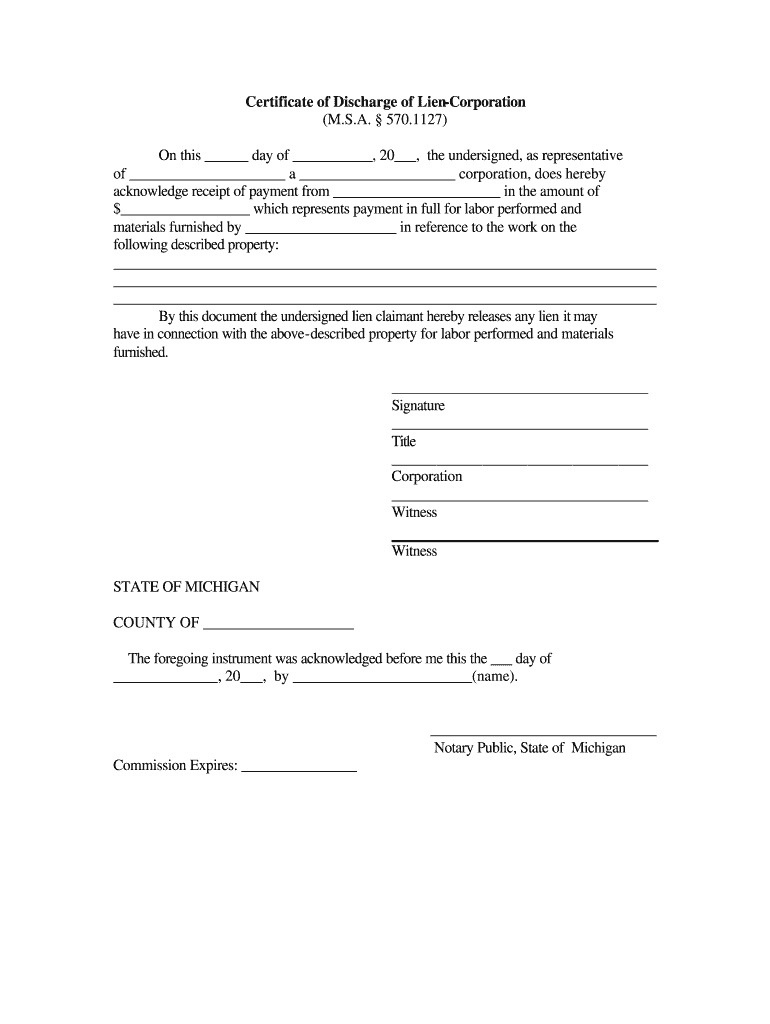
Application for Discharge Certificate Form Fill Out and Sign Printable PDF Template signNow
Hospital Discharge Paper is used to show that patient was discharge from hospital or clinic after treatment and rest. FILL ONLINE EMAIL SHARE ANNOTATE FILL ONLINE FILL ONLINE Contents What is Hospital Discharge Paper How to fill out Hospital Discharge Paper FAQs about Hospital Discharge Paper How to Get and Edit Hospital Discharge Paper template Your discharge planner can tell you why you are going home or to another health care setting and why your care is changing. You will work together on: What care and services you may need after you leave. This can include nursing, physiotherapy, occupational therapy, or speech therapy. In order to ensure this, hospital management usually has a form which they fill and check in before discharging a patient. In our world today where people are using less of paper, this hospital discharge template is one PDF document you can use to save patient discharge information. In a large retrospective cohort study conducted in the United States, patients with an AMA discharge were more likely to experience 30-day hospital readmission compared with routine discharge (25.6 versus 11.5 percent), and AMA discharge was an independent predictor of readmission across a wide range of diagnoses [ 97 ].
FREE 14+ Sample Discharge Summary Templates in MS Word PDF
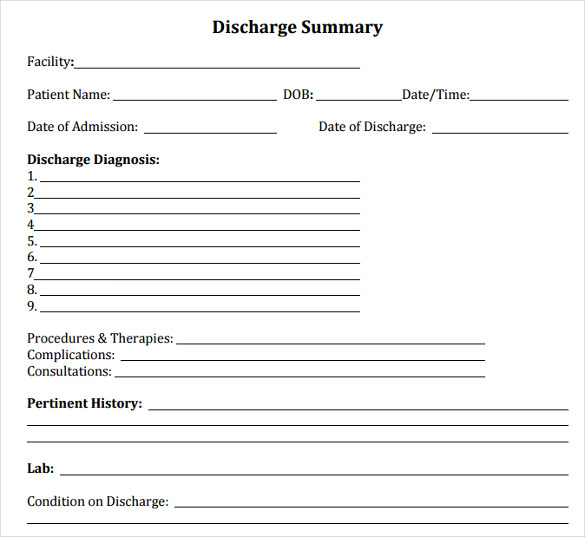
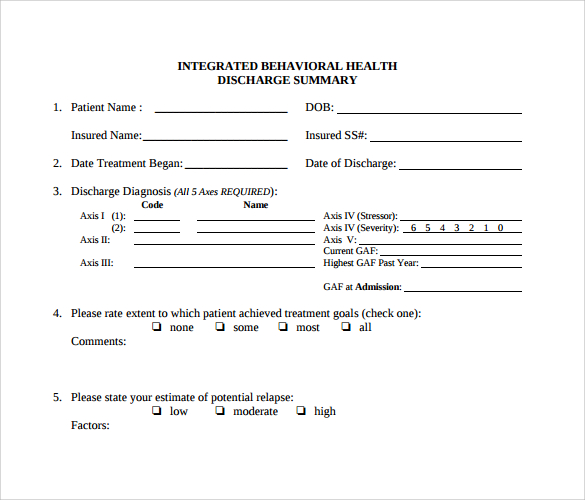
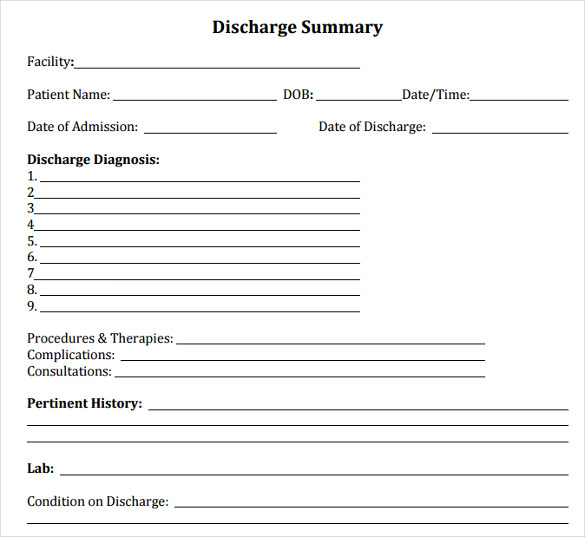
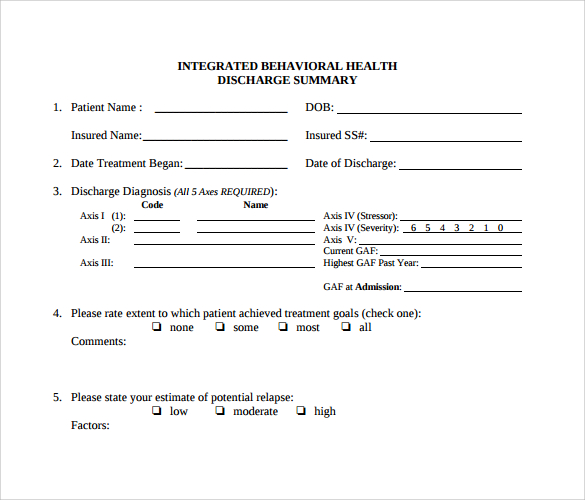
A discharge summary is a clinical report prepared by a health professional at the conclusion of a hospital stay or series of treatments. It is often the primary mode of communication between the hospital care team and aftercare providers. It is considered a legal document and it has the potential to jeopardize the patient's care if errors are made. Introduction. Public health agencies and researchers rely heavily on birth certificate and hospital discharge data for national and local surveillance and research activities related to pregnancy complications, risk behaviors, and neonatal outcomes [1, 2].These data sources are large, accessible, and available for nearly all in-hospital births in the United States. Introduction. Hospital discharge summaries serve as the primary documents communicating a patient's care plan to the post-hospital care team. 1, 2 Often, the discharge summary is the only form of communication that accompanies the patient to the next setting of care. 1 High-quality discharge summaries are generally thought to be essential for promoting patient safety during transitions. Adding hospital discharge data changed the underlying cause in 11% of deaths. For some causes of death, including medical misadventures and accidental falls, the effect was substantial. Conclusion: Most differences between underlying cause of death and final main condition can be explained by differences in ICD selection procedures.
FREE 14+ Sample Discharge Summary Templates in MS Word PDF
Hospital Discharge Documentation. Prepare the necessary documentation, including a summary of the patient's stay, diagnoses, treatment received, medications prescribed, and any relevant instructions. Ensure that the discharge summary is accurate, and complete, and includes contact information for the healthcare team involved in the patient's care. Discharge summary forms are usually completed during a patient's hospital stay and contain essential medical information about the care they received, including details about allergies, medications, and clinical findings. This document facilitates continuity of care for patients.
This chapter reviews the two literatures that inform this study. The first addresses the safety challenge of hospital discharge, elaborating this as a problem of co-ordination and collaboration among various health and social care agencies. Hospital Discharge Summary 1 Obtain preliminary report from the attending physician Compile patient medical records and treatment details Draft a preliminary discharge summary Approval: Physician's Review of Preliminary Discharge Summary Incorporate review feedback into the discharge summary Complete additional medical documentation as required

Hospital Discharge form Template Beautiful Best S Of Hospital Discharge Papers Printable Pdf
A doctor who decided the discharge of the patient and who treated the patient during a hospital stay is only authorized to fill out the form and precedes it to the billing department through the nursing staff. Components of a patient discharge form Get hospital discharge certificate and then click Get Form to get started. Take advantage of the instruments we offer to submit your document. Highlight relevant paragraphs of your documents or blackout sensitive information with instruments that signNow offers specifically for that function.