13 Blank SBAR Templates (Word, PDF) SBAR is an acronym for Situation, Background, Assessment, Recommendation. It is a technique used to facilitate appropriate and prompt communication. An SBAR template will provide you and other clinicians with an unambiguous and specific way to communicate vital information to other medical professionals. What Is SBAR Used For in Nursing? SBAR can be used to communicate information between healthcare professionals, i.e., from nurse to physician or allied healthcare professional, as well as when relaying information to a patient or their caregivers.

Sbar Nursing Report Template kulturaupice
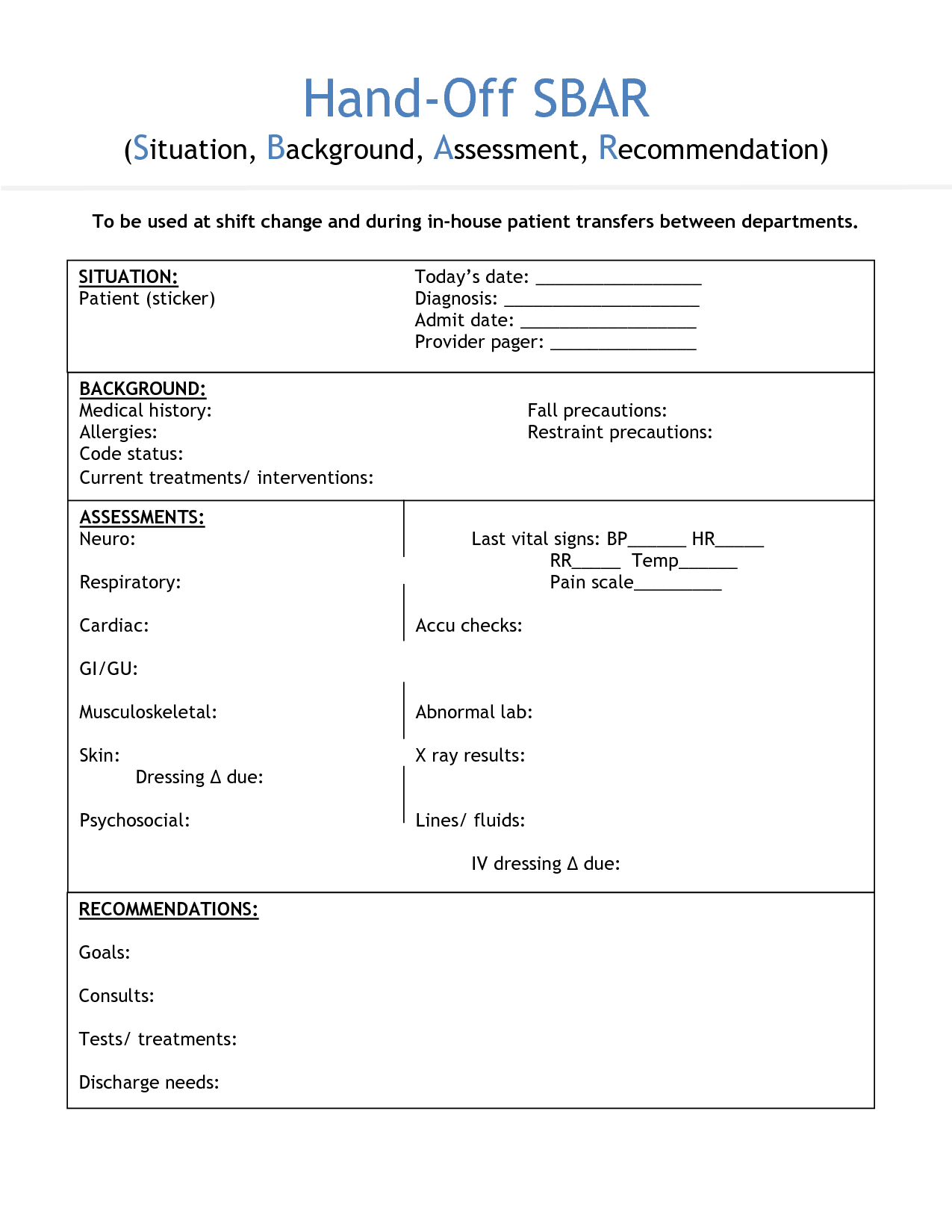
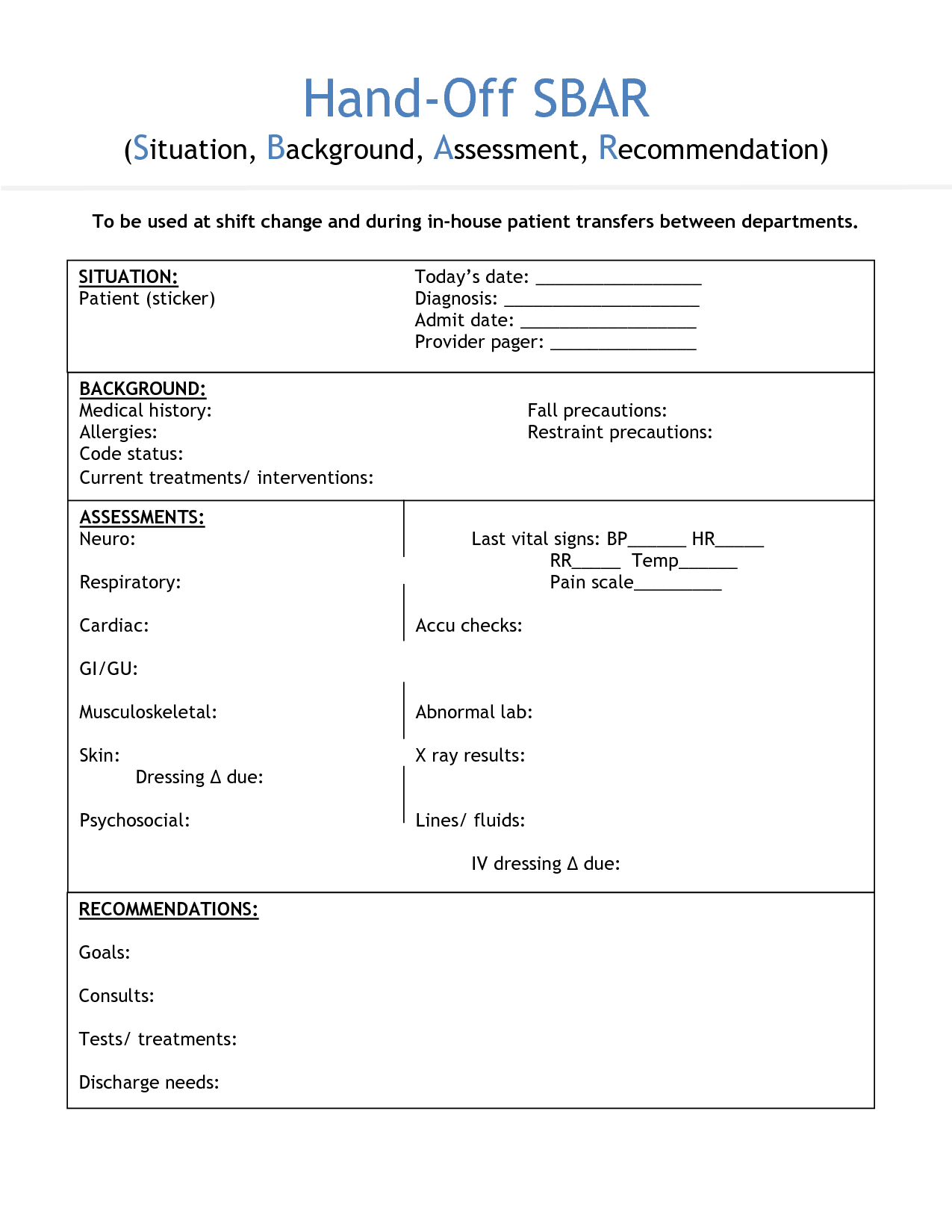
An SBAR Nursing Template provides a structured framework through which nursing professionals can communicate effectively about a patient's status and needs with other healthcare team members, ensuring clarity, succinctness, and a systematic approach to sharing critical information. An SBAR report is a tool of communication between members of the healthcare team about a client's condition that follows the SBAR communication technique. SBAR stands for: S ituation B ackground A ssessment R ecommendation What is the purpose of the SBAR technique? Example #3: Night Nurse Giving SBAR Report to Oncoming Nurse for Patient Admitted During the Overnight Shift • Situation: "Mrs. Thomas, in room 316, is an 84-year-old female admitted last night at 2230. She arrived at the emergency rule via ambulance from Magnolia Nursing Home where she reportedly fell trying to go to the restroom. Background In the background section of our nurse report sheet, we want to give a general overview of our patient's history so the incoming nurse can get a better idea of who our patient is and anticipate her needs. SBAR is about being relevant and straight to the point so we do not need to share our patient's (Pat) entire medical history.
free sbar template for nurses Sbar Report Sheet Template Nurse report
FOR NURSING STUDENTS (Giving report while you are in school & to your professors!) Email me the FREE Printable Report Sheet Your Info Is 100% Safe. If you have issues downloading, please email
[email protected] Printable Nursing Report Sheet allows you to: Discover how easy giving report can be. 🎉 Always know what to say. The SBAR (Situation-Background-Assessment-Recommendation) technique provides a framework for communication between members of the health care team about a patient's condition. SBAR is an easy-to-remember, concrete mechanism useful for framing any conversation, especially critical ones, requiring a clinician's immediate attention and action. What is the nurse's recommendation or what does he/she want? Physician follow-up actions are suggested, including possible tests. Examples: Notification that patient has been admitted Patient needs to be seen now Order change Guidelines for Communicating with Physicians Using the SBAR Process 1. What is SBAR? It's a communication method used to promote and simplify communicating important patient information to other members of the healthcare team. The SBAR method strategically helps communicate a specific patient situation along with the patient's background, your assessment, and possible recommendations.
Single Patient Nurse Report Sheet template Sbar & Brain Nursing Report
What is the SBAR technique in nursing? In nursing, the situation, background, assessment and recommendation (SBAR) technique is a tool that allows health professionals to communicate clear elements of a patient's condition. SBAR stands for Situation, Background, Assessment, and Recommendation. This method is used to organize and communicate important patient information in a structured and concise manner. The SBAR method is commonly used in nursing to communicate critical information between nurses, physicians, and other healthcare providers.
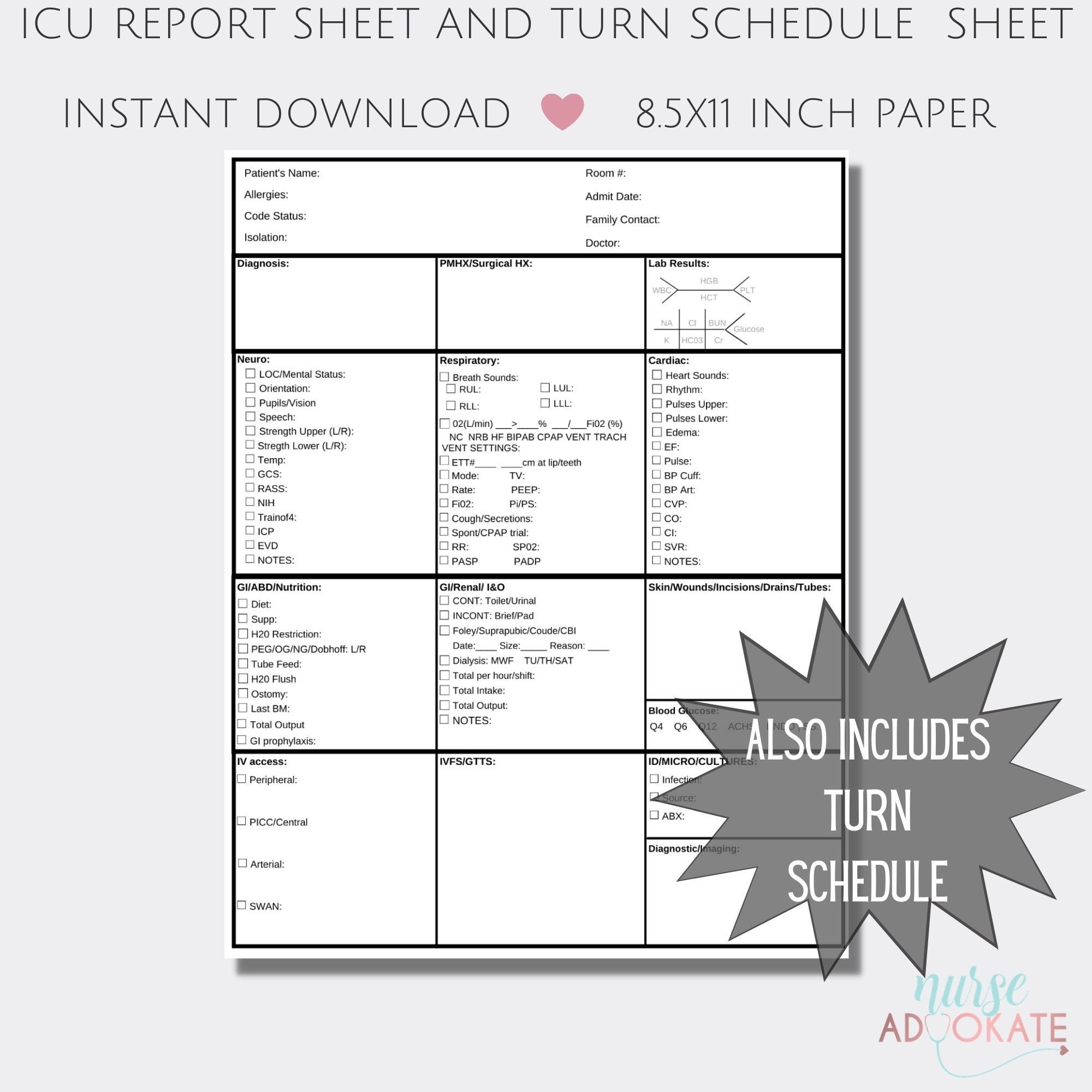
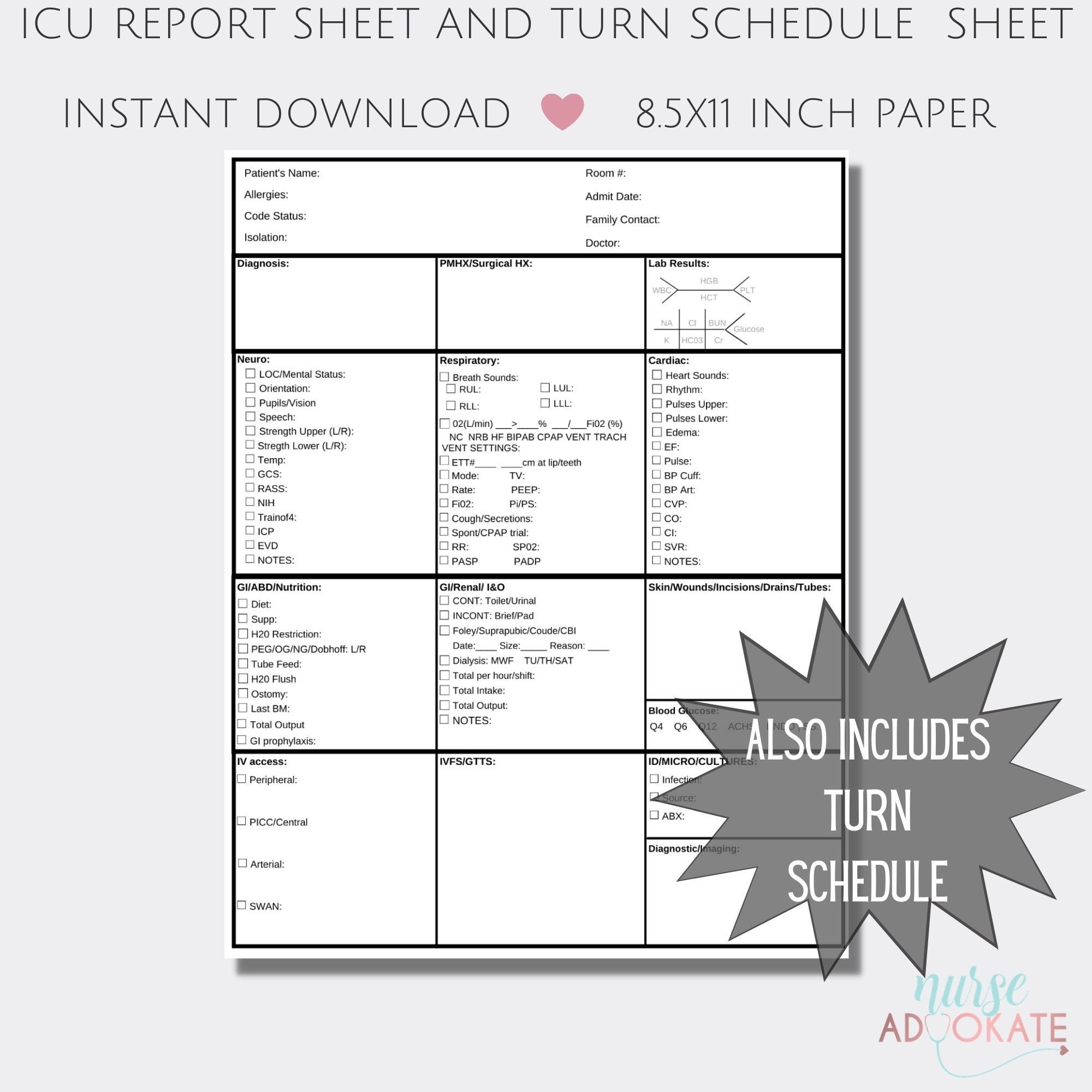
Free downloadable tools to support your work to improve health care quality and safety at every stage — from establishing a project plan and an improvement aim, to understanding a process, to identifying root causes or drivers, to testing changes using PDSA cycles, to implementing and spreading successful improvements, and more. Featured Tools Nursing Brainsheets vs SBAR. Keep in mind that a nursing report sheet is different from an SBAR tool (situation, background assessment, recommendation tool). An SBAR tool includes important health history, an assessment of the patient's current state, a briefing of recommended action, and so on..

Image result for sbar report sheet for nurses NURSING Pinterest
The Ultimate Nurse Report Sheet Helping nurses spend more time with patients & less on busywork Download Now Learn More Streamlined Nursing You didn't become a nurse to spend half your shift in front of a computer. NurseBrain fixes this by automating your charting and organizing your patient info & tasks in one convenient place. What are Nursing Report Sheets? Nursing report sheets are standardized forms used to document a patient's condition, including vital signs, medications, treatments, and any relevant observations. They serve as a communication tool between nurses, ensuring continuity of care throughout the patient's journey. Benefits of Using Nursing Report Sheets: